America’s addiction crisis continues unabated. Last year, more than 107,000 Americans died of drug overdoses, setting another tragic record in the nation’s escalating overdose epidemic, according to an estimate published by the Centers for Disease Control and Prevention (CDC) in May.
The provisional 2021 data translates to roughly one US overdose death every 5 minutes and marked a 15 percent increase from the previous record, set only the year before. The director of the National Institute on Drug Abuse, Nora Volkow, called the latest numbers “truly staggering.”
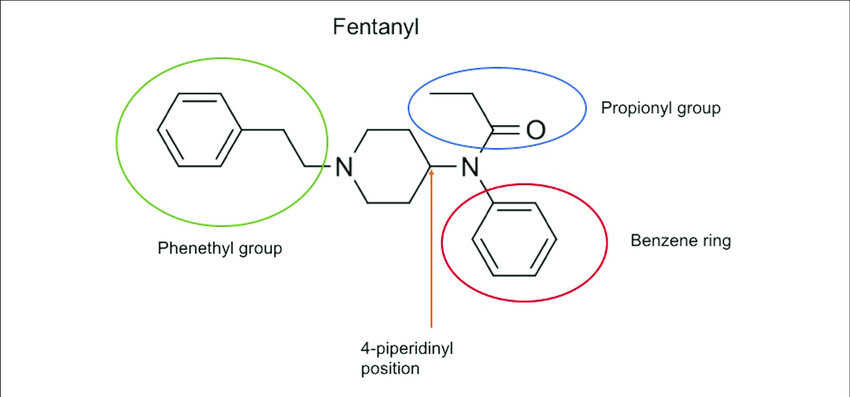
US overdose deaths have risen most years for more than two decades. The increase began in the 1990s with overdoses driven by the misuse of opioid painkillers, followed by waves of deaths led by other opioids like heroin and—most recently—illicit fentanyl, a synthetic opioid that can easily be mass-produced in laboratories.
Many people with addiction misuse multiple drugs and the inexpensive fentanyl has increasingly been cut into other drugs, often without users being aware of that.
Fentanyl is not only cheap to manufacture but also extremely potent. The synthetic opioid is up to 80 times more powerful than morphine. Last year, overdoses involving fentanyl and other synthetic opioids surpassed 71,000, up 23 percent from the year before. There also was a 23 percent increase in deaths involving cocaine and a 34 percent increase in deaths involving meth and other stimulants.
Fentanyl misuse is not only more lethal, but it is also more complicated to treat than addiction to other opioids. Fentanyl is highly lipophilic—i.e. easily stored in fat cells—and “with regular use may become sequestered in adipocytes (fat cells) or other tissues, leading to prolonged clearance,” wrote Darius Rastegar, MD on a Boston University health page.
When researchers serially tested the urine of 12 participants with opioid use disorder (OUD) in a 28-day residential program who tested positive for fentanyl, they found that the mean time for clearance of fentanyl was seven days and norfentanyl (a metabolite) 13 days after last use. One participant continued to test positive for fentanyl for 19 days and norfentanyl 26 days after last use.
This “may have implications for treatment of individuals with opioid use disorder and may explain reports of difficulties with initiation of buprenorphine due to precipitated withdrawal in individuals using fentanyl,” Dr. Rastegar concluded. “We need more research on optimizing buprenorphine initiation for individuals with fentanyl use and investigations of alternative approaches.”
Buprenorphine, methadone, and naltrexone are the three FDA-approved medications used to treat addiction to opioids such as heroin, morphine, and codeine, and semi-synthetic opioids like oxycodone and hydrocodone, as well as synthetic opioids such as fentanyl.
Huhn, Hobelmann, Oyler, and Strain made similar observations in their 2020 study on the renal clearance of fentanyl in persons with opioid use disorder.
“Fentanyl clearance in persons with OUD is considerably longer than the typical 2–4 day clearance of other short-acting opioids. The findings of this study might explain recent reports of difficulty in buprenorphine inductions for persons who use fentanyl, and point to a need to better understand the pharmacokinetics of fentanyl in the context of opioid withdrawal in persons who regularly use fentanyl.”
The high lipophilicity of fentanyl is similar to persons who use marijuana regularly and experience protracted renal clearance of tetrahydrocannabinol (THC), the main psychoactive substance in cannabis (marijuana). Some THC metabolites have an elimination half-life of 20 hours whereas others are stored in body fat and have an elimination half-life of 10–13 days
“Protracted fentanyl clearance might also extend opioid withdrawal and post-withdrawal sequalae, changing the length and trajectory of acute care for persons undergoing supervised withdrawal,” wrote Huhn, Hobelmann, et al. “Fentanyl clearance may take several weeks for persons with OUD who are exposed to fentanyl on a daily basis… and treatment providers should be aware that clearance of fentanyl is fundamentally different than other opioids and can have serious negative implications during early OUD treatment.”
Detoxification from opioid poisoning is complicated and should be supervised by medical professionals. Detox is not a cure and marks only the first treatment stage in a continuous recovery journey. Valiant Living Detox and Assessment provides comprehensive care beyond withdrawal management to launch a life-changing recovery from addiction.
We offer a transitional short-term residential program to make it easier for clients to consider the best way forward after medical detox. The program helps clients and their families understand often unfamiliar treatment options better. Its emphasis is on post-detox stabilization and it prioritizes treatment planning and next-step care coordination.
At Valiant Living Detox and Assessment, we do more than safely detoxify. If you are seeking a more comprehensive start for your treatment of addiction, contact us at 303-647-4932. We provide a safe, supportive haven in the earliest stages of recovery. Get the individualized attention you need for stabilization, assessment, and discerning the best next steps in your journey.